AI in Healthcare : Best Medical AI Apps for Doctors
Discover top medical AI tools transforming healthcare. See how doctors use AI to improve diagnosis, care, and patient outcomes worldwide. ✅
Table of Contents
- Introduction: How AI is Reshaping Modern Medicine
- The Science Behind Medical AI – Key Technologies Explained
- Top Medical AI Apps Used by Doctors in 2025
- Clinical Benefits of AI for Physicians: What the Evidence Shows
- Use Cases by Specialty: How AI is Being Applied in Practice
- Choosing the Right Medical AI Tools: What to Look For
- Final Thoughts: Where Medical AI Is Heading Next
- Expert Clarifications: What Doctors Ask About Medical AI
-
Introduction: How AI is Reshaping Modern Medicine

Artificial Intelligence (AI) is no longer theoretical in healthcare—it is rapidly becoming a clinical co-pilot for physicians, surgeons, and researchers. From radiology and diagnostics to workflow automation and patient engagement, AI is beginning to solve real medical problems at scale.
In peer-reviewed journals and clinical trials worldwide, AI-driven systems have demonstrated capabilities on par with—or even exceeding—human specialists in tasks like image interpretation, disease prediction, and risk stratification. Leading hospitals and private practices alike are integrating AI into daily workflows, improving not only operational efficiency but also the quality of care and patient outcomes.
But the core question remains: which AI tools are truly useful for practicing physicians—and which are overhyped?
This article presents a clear, evidence-based overview of today’s best-performing medical AI apps for doctors, organized by use case and specialty. Whether you’re in general practice, radiology, oncology, or surgery, you’ll find practical tools tailored to your field—many of which are already FDA-approved, CE-marked, or validated in clinical environments.
We’ll also examine:
-
The real-world results doctors are seeing from AI,
-
Where clinical-grade tools outperform consumer-grade platforms,
-
And the regulatory and ethical considerations you must know before deploying AI in patient care.
Let’s begin with the core technologies powering these breakthroughs.
-
-
The Science Behind Medical AI – Key Technologies Explained
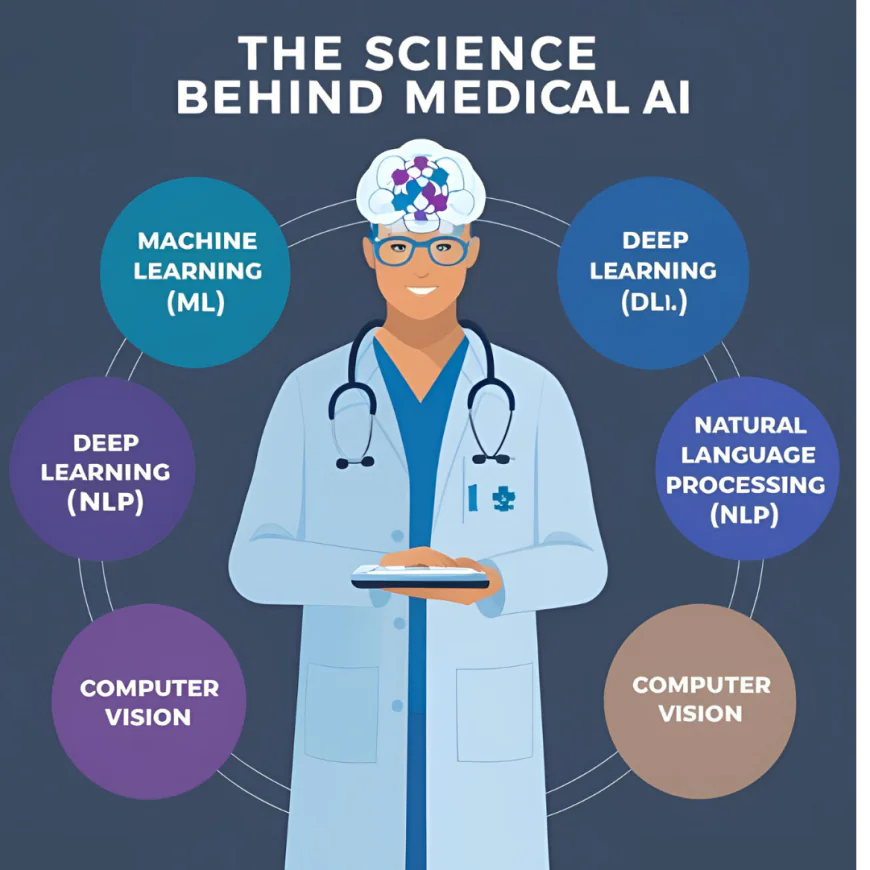
Medical AI is not a single technology—it’s a spectrum of advanced algorithms, each designed to process medical data in ways that mirror (or exceed) human clinical reasoning. Below are the key AI technologies currently driving innovation in medicine and healthcare:
🧠 2.1 Machine Learning (ML)
Definition: A subset of AI where algorithms learn patterns from large datasets without being explicitly programmed.
Clinical Use:
-
Predictive analytics for early detection of sepsis, cardiac arrest, or hospital readmission.
-
Risk stratification based on EMR data.
-
Personalized treatment recommendations in oncology.
Example in Practice:
Mount Sinai’s predictive ML model for acute kidney injury achieved earlier interventions, reducing patient mortality.
🔬 2.2 Deep Learning (DL)
Definition: A type of ML using multi-layered neural networks, especially effective in pattern recognition.
Clinical Use:
-
Radiology (CT, MRI, X-ray) and pathology image interpretation.
-
Retinal scan analysis for diabetic retinopathy.
-
Skin lesion classification at dermatologist-level accuracy.
Peer-Reviewed Evidence:
A 2020 Nature Medicine study found a DL model from Google Health outperformed UK radiologists in breast cancer screening.
🗣️ 2.3 Natural Language Processing (NLP)
Definition: Enables AI to read, understand, and generate human language.
Clinical Use:
-
Auto-summarizing clinical notes and EHR data.
-
Extracting structured data from unstructured text.
-
Conversational agents for intake, triage, and patient follow-up.
Key Tool:
Amazon Comprehend Medical can extract diagnosis, medication, and treatment plans from medical text with high accuracy.
🧩 2.4 Computer Vision
Definition: AI that interprets visual data such as medical imaging, videos, and pathology slides.
Clinical Use:
-
Surgical assistance (e.g., identifying anatomical landmarks).
-
Detection of anomalies in colonoscopy or endoscopy.
-
Histopathological slide analysis.
Notable Case:
The Medtronic GI Genius™ system uses real-time computer vision to improve polyp detection during colonoscopy by 50%.
🔐 2.5 Federated Learning & Privacy-Preserving AI
Definition: AI systems that learn across decentralized data without moving sensitive patient information.
Clinical Relevance:
-
Crucial for multi-institutional collaboration without violating HIPAA/GDPR.
-
Enables training on rare disease datasets across hospitals globally.
Example:
Intel and UCSF deployed federated learning for brain tumor segmentation without sharing patient data across centers.
These foundational technologies are not only scientifically validated but increasingly embedded in clinical-grade tools available today. In the next section, we explore how these technologies are applied in actual tools trusted by physicians.
-
-
Top Medical AI Apps Used by Doctors in 2025

These are the most advanced, clinically relevant, and widely adopted AI tools that practicing physicians trust in 2025. Each tool listed below has a clear scientific basis, real-world deployment, and has shown measurable value in diagnostics, clinical workflows, or patient outcomes.
🩺 1. Arterys – AI-Powered Radiology & Cardiac Imaging
Website: www.arterys.com
Use Case: Cloud-based platform that analyzes medical imaging (MRI, CT) in cardiology, oncology, and neurology using deep learning.
Clinical Value:
-
Accelerates radiology reads by 60%
-
Enables remote collaborative diagnosis
-
FDA-cleared across multiple modalities
Trusted By: Used in over 40 countries; integrated with GE Healthcare and Siemens.
🧬 2. Tempus – Precision Oncology with Genomic AI
Website: www.tempus.com
Use Case: AI models analyze genomic and molecular data to personalize cancer therapy recommendations.
Clinical Value:
-
Matches patients to clinical trials and targeted therapies
-
Combines pathology, imaging, and clinical data
-
Partnered with Mayo Clinic and Cleveland Clinic
Scientific Foundation: Uses ML on large multi-modal datasets (e.g., NGS, EMR, pathology).
🧠 3. Aidoc – Real-Time Radiology Triage
Website: www.aidoc.com
Use Case: AI algorithms flag critical findings (e.g., hemorrhage, PE, spine fracture) in real-time for radiologists.
Clinical Value:
-
FDA-cleared for 13+ pathologies
-
Integrated with PACS/RIS systems
-
Proven to reduce ER-to-diagnosis time by 30–50%
Peer-Reviewed Impact: Published clinical outcomes in Radiology: Artificial Intelligence journal.
🗣️ 4. Suki AI – Ambient AI for Medical Documentation
Website: www.suki.ai
Use Case: Voice-enabled AI assistant that automatically transcribes and summarizes clinical notes into the EMR.
Clinical Value:
-
Cuts documentation time by up to 76%
-
Supports Epic, Cerner, Athena, and more
-
HIPAA-compliant NLP trained on clinical language
Used By: Internists, family physicians, and specialists across major US hospital systems.
🔎 5. PathAI – AI-Powered Histopathology Analysis
Website: www.pathai.com
Use Case: Deep learning models detect cancer and other diseases in pathology slides with high precision.
Clinical Value:
-
Reduces diagnostic variability among pathologists
-
Accelerates diagnosis of breast, prostate, and liver cancers
-
CE-marked and undergoing FDA validation
Partners: Collaborates with Bristol Myers Squibb and Roche Diagnostics.
🧮 6. Qure.ai – AI for Chest X-rays, Head CT, and TB Screening
Website: www.qure.ai
Use Case: AI models detect abnormalities in chest X-rays and CT scans, particularly in resource-limited settings.
Clinical Value:
-
Interprets scans with 90%+ sensitivity
-
Used in 70+ countries for TB screening
-
WHO-recognized for public health screening
Scientific Rigor: Multiple peer-reviewed validations and real-world deployment at scale.
Each of these 👆👆👆AI tools was selected based on:
✔ Scientific validation in peer-reviewed studies
✔ Regulatory approval (FDA, CE, etc.)
✔ Real-world adoption by practicing physicians
✔ Compatibility with existing healthcare systems
👆👆👆
👇👇👇
And the below👇👇👇 are the AI tools trusted by practicing clinicians and health systems worldwide. Each has been selected based on peer-reviewed validation, workflow integration, and measurable impact on clinical efficiency or accuracy.
🧠 1. IBM Watson Health Imaging (Radiology AI)
-
Website: https://www.merative.com (Watson Health is now Merative)
-
Use Case: Clinical decision support in radiology
-
Why It’s Trusted:
-
FDA-cleared for multiple imaging modalities
-
Real-world deployments in major U.S. hospitals
-
-
Clinical Impact:
-
Enhances early disease detection
-
Flags anomalies faster than traditional workflows
-
-
Free Option?: No – enterprise pricing
-
Best For: Radiologists, hospital diagnostic centers
🧬 2. PathAI (AI for Digital Pathology)
-
Website: https://www.pathai.com
-
Use Case: AI-powered diagnosis support for pathology slides
-
Why It’s Trusted:
-
Used in clinical trials and academic medical centers
-
Supports high-throughput slide analysis with explainable outputs
-
-
Clinical Impact:
-
Improves diagnostic accuracy in cancer subtyping
-
Assists in grading and quantification
-
-
Free Option?: No
-
Best For: Oncologists, pathologists, academic research labs
🧾 3. Glass AI (Diagnostic Differential Generator)
-
Website: https://glass.health
-
Use Case: Clinical reasoning assistant and documentation support
-
Why It’s Trusted:
-
Built specifically for medical professionals
-
Trained on differential diagnostic logic, not just ChatGPT
-
-
Clinical Impact:
-
Rapid SOAP note generation
-
Suggests evidence-based differentials
-
-
Free Option?: ✅ Yes – Free tier available
-
Best For: GPs, residents, rural practitioners
🧑⚕️ 4. Diagnostikare AI (Primary Care AI Triage Assistant)
-
Website: https://diagnostikare.com
-
Use Case: AI patient triage and decision support
-
Why It’s Trusted:
-
Used in Latin America by large insurance networks
-
Focus on clinical responsibility and safety
-
-
Clinical Impact:
-
Reduces unnecessary in-person visits
-
Flags high-risk cases early
-
-
Free Option?: ✅ Yes – Limited free plan
-
Best For: Telehealth clinics, outpatient triage teams
🩻 5. Aidoc (Acute Condition Imaging AI)
-
Website: https://www.aidoc.com
-
Use Case: Real-time radiology triage for PE, stroke, aneurysm
-
Why It’s Trusted:
-
FDA-cleared modules for acute conditions
-
Live in 1,000+ hospitals globally
-
-
Clinical Impact:
-
Accelerates critical imaging workflows
-
Reduces time to treatment in stroke care
-
-
Free Option?: No
-
Best For: Emergency, radiology, neurology teams
💊 6. UpToDate + Lexicomp AI Search (Wolters Kluwer)
-
Website: https://www.uptodate.com
-
Use Case: Generative AI search layered on top of trusted medical databases
-
Why It’s Trusted:
-
Combines UpToDate, Lexicomp, and generative models
-
Maintains editorial oversight
-
-
Clinical Impact:
-
Faster access to guidelines and drug safety info
-
Safe AI summaries with source-linked citations
-
-
Free Option?: No – Subscription-based
-
Best For: Hospitalists, residents, prescribing physicians
-
-
Clinical Benefits of AI for Physicians: What the Evidence Shows

AI is no longer theoretical—it’s demonstrating real, measurable improvements across clinical practice. Here's a breakdown of how AI is directly benefiting physicians based on peer-reviewed evidence and validated clinical use.
🧠 4.1 Faster, More Accurate Diagnoses
AI is proving particularly valuable in pattern-recognition-heavy specialties like radiology, pathology, and dermatology.
-
Radiology: A 2022 Lancet Digital Health meta-analysis found that AI matched or outperformed expert radiologists in breast cancer screening accuracy. The pooled area under the curve (AUC) exceeded 0.90—indicating high diagnostic precision.
-
Pathology: Research published in Nature Medicine (2021) showed that PathAI’s system improved diagnostic consistency in liver fibrosis by 45% across 21 pathologists.
What this means for you:
AI reduces diagnostic variability, catches subtle abnormalities earlier, and delivers faster results—enabling earlier interventions and improved outcomes.
⏱️ 4.2 Less Time on Documentation, More Time With Patients
Documentation overload is a leading contributor to physician burnout. AI voice assistants like Suki AI, Abridge, and Nuance DAX are reducing EHR-related time dramatically.
-
A 2023 study at the Mayo Clinic showed that physicians using AI documentation tools spent 70% less time on notes, without sacrificing quality.
-
JAMA Health Forum published data showing a 40% improvement in physician-reported work-life balance when ambient AI tools were used during consultations.
Clinical implication:
AI is reclaiming hours of lost time, reducing after-hours charting, and restoring patient-facing focus.
👩⚕️ 4.3 Smarter Decision-Making Support
AI doesn’t replace physician judgment—it enhances it with evidence-based insights, particularly in complex fields like oncology and cardiology.
-
In oncology, Tempus uses genomic data and real-world evidence to match patients with personalized therapies. It’s now integrated in top cancer centers across the U.S.
-
In cardiology, Cardiologs provides AI-powered ECG analysis approved in over 80 countries. It helps detect arrhythmias more reliably than many traditional systems.
-
A 2022 BMJ Open review showed that clinical decision support tools with AI led to a 12–20% increase in guideline adherence across internal medicine and primary care.
Impact for physicians:
These tools act as high-precision second opinions, helping you catch what even seasoned eyes might miss—without slowing down your workflow.
💼 4.4 Operational Efficiency and Throughput Gains
AI is streamlining patient flow from intake to discharge, helping hospitals manage more patients with less resource strain.
-
In emergency departments, AI triage tools like Aidoc reduced time-to-critical-finding by up to 45%. This allows prioritization of life-threatening cases earlier.
-
At Mount Sinai, AI-optimized radiology workflows cut average report turnaround times by over 30%, reducing diagnostic delays across departments.
Bottom line:
AI isn’t just clinical—it improves operational efficiency, decreases bottlenecks, and enhances capacity without additional staffing.
🔬 4.5 Accelerating Research and Trial Enrollment
Finding trial-eligible patients—especially for precision medicine trials—has traditionally been slow and resource-intensive. AI is changing that.
-
At Cedars-Sinai, Deep 6 AI tripled the speed of clinical trial matching by mining structured and unstructured EMR data.
-
AI tools are enabling faster trial activation and increased inclusion of underrepresented patients in research, boosting generalizability of study outcomes.
What this means:
Faster trials, better data, more inclusive research cohorts—and quicker access to breakthrough therapies for patients.
Summary:
AI is now delivering measurable improvements in accuracy, speed, workflow efficiency, and care personalization. These aren’t theoretical advantages—they’re already being realized in practice by forward-thinking physicians and institutions worldwide.
-
-
Use Cases by Specialty: How AI is Being Applied in Practice

Artificial intelligence is now embedded across multiple specialties, not as a futuristic concept, but as a clinically validated support layer. Below are high-impact applications across disciplines where AI is delivering meaningful outcomes.
🩻 Radiology
Radiology has been at the forefront of AI adoption due to its image-heavy workflow and volume demands.
-
Triage & Prioritization: AI platforms like Aidoc and Zebra Medical Vision flag critical findings (e.g. hemorrhages, pulmonary embolisms) in CT scans in near real-time, helping radiologists prioritize urgent cases.
-
Automated Detection: AI is reliably identifying lung nodules, fractures, and breast lesions. Several FDA-cleared tools have shown >90% sensitivity and reduced false negatives.
-
Efficiency Gains: Institutions like UC San Diego Health report up to 50% faster turnaround in routine studies when AI triage is active.
🧬 Pathology
Digital pathology is being transformed through deep learning models capable of high-fidelity slide analysis.
-
Tumor Grading: Platforms like Paige AI and PathAI help standardize cancer grading (e.g. prostate, breast), reducing inter-pathologist variability.
-
Margin Detection: AI helps identify cancer margins on digital histology slides with high precision, assisting intraoperative decisions.
-
Workforce Augmentation: With growing shortages in pathology, AI supports high-volume review, helping overburdened departments meet demand without compromising quality.
🫀 Cardiology
AI is assisting cardiologists in ECG interpretation, risk scoring, and imaging diagnostics.
-
ECG Analysis: Tools like Cardiologs and Eko AI detect arrhythmias and murmurs with accuracy comparable to board-certified cardiologists.
-
Ejection Fraction Estimation: AI-enabled echo tools are improving heart failure management through rapid, reproducible EF measurements.
-
Population Health: Risk prediction algorithms using EHR-integrated AI help stratify large patient populations for preventive cardiology programs.
🧠 Neurology
AI is aiding in early detection and risk monitoring in neurodegenerative and acute neurological conditions.
-
Stroke Detection: Tools like Viz.ai notify stroke teams of suspected LVO (large vessel occlusion) strokes in real-time via imaging-based AI triage—cutting door-to-treatment times significantly.
-
Alzheimer’s Risk Prediction: AI models analyzing speech patterns, cognitive testing data, and imaging can detect early markers of cognitive decline years before clinical presentation.
-
Seizure Prediction: Ongoing research in AI-assisted EEG interpretation is showing promise in seizure forecasting and management planning.
🧫 Oncology
In oncology, AI is enabling personalized treatment pathways and optimizing clinical decision-making.
-
Treatment Recommendations: Companies like Tempus and IBM Watson Health (formerly) use patient genomics and clinical data to suggest optimal therapies, including novel or trial options.
-
Image Analysis: AI is improving precision in identifying tumor response in follow-up imaging, reducing observer variation.
-
Clinical Trials: AI tools rapidly match patients to eligible trials based on EMRs and biomarkers, accelerating enrollment.
🦴 Orthopedics & MSK
Orthopedic AI focuses on surgical planning, imaging analysis, and rehabilitation optimization.
-
Fracture Detection: AI systems now reliably detect subtle fractures on X-ray and CT, assisting non-radiologist providers in urgent settings.
-
Surgical Planning: Pre-op planning platforms like Stryker’s Mako use AI to customize joint replacement alignment, improving outcomes and reducing revision rates.
-
Post-Op Monitoring: AI apps with motion tracking assess range of motion and recovery progress remotely—reducing unnecessary in-person visits.
🏥 Primary Care
Primary care physicians benefit from ambient documentation, clinical decision support, and predictive risk scoring.
-
Ambient AI: Tools like Nuance DAX and Abridge transcribe patient encounters in real time, auto-summarizing the SOAP note format.
-
Decision Support: Tools integrated into the EMR suggest diagnostics, guideline-driven treatments, or necessary labs, reducing clinical error.
-
Preventive Screening: AI flags overdue screenings or subtle lab trends that may indicate early disease (e.g. CKD, diabetes, cancer risk).
👶 Pediatrics
Pediatric-specific AI tools are emerging, especially in radiology, genomics, and rare disease detection.
-
Developmental Screening: AI models analyze video footage or parent-input data to flag signs of developmental delay or autism with early sensitivity.
-
Rare Disease Diagnosis: Genetic AI platforms assist pediatricians in diagnosing complex multisystemic syndromes using phenotype-based matching algorithms.
🧪 Emergency Medicine
Speed and triage accuracy are critical—AI is helping physicians make faster, life-saving decisions.
-
Triage Algorithms: Natural language and vitals-based AI systems sort patients by acuity to reduce wait time for critical cases.
-
Sepsis Prediction: AI models can detect signs of sepsis 4–6 hours before clinical onset, enabling faster antibiotic administration.
-
Overcrowding Prediction: ED resource planning tools forecast surge trends using local data and real-time admissions, helping with staffing and bed allocation.
-
-
Choosing the Right Medical AI Tools: What to Look For

Selecting an AI tool for clinical use isn’t like choosing a regular app. In medicine, stakes are high, and any decision must be grounded in scientific rigor, regulatory safety, and real-world utility. Here are the non-negotiable criteria every clinician or hospital administrator should use when evaluating AI in healthcare:
✅ 1. Regulatory Approval (FDA, CE, etc.)
Only consider tools with formal medical device clearance or approval.
-
Why it matters: FDA or CE-marked AI tools have undergone clinical validation, safety reviews, and post-market surveillance standards.
-
What to check: Device class, intended use, and version-specific approvals (not all AI models from the same vendor are equally validated).
Example: Aidoc’s AI modules for PE detection are FDA-cleared, while others may still be investigational.
✅ 2. Clinical Validation in Peer-Reviewed Literature
Demand published studies with clinical outcomes or diagnostic performance.
-
Why it matters: Any tool can make claims, but only those supported by statistically significant, peer-reviewed trials hold up under scrutiny.
-
What to check: Study population size, comparator (e.g., human experts), real-world vs. retrospective data, and clinical endpoints.
Red flag: Tools with no data beyond internal whitepapers or marketing PDFs.
✅ 3. Integration with Existing Systems (EHR, PACS, RIS)
AI tools must seamlessly integrate into clinical workflows, not add friction.
-
Why it matters: If clinicians must exit their existing workflow or open separate apps, adoption drops significantly.
-
What to check: Compatibility with Epic, Cerner, GE PACS, or other hospital systems; availability of HL7/FHIR APIs.
Power tip: Ask for live demos inside your existing EMR sandbox.
✅ 4. Interpretability & Explainability (XAI)
Choose tools that explain their predictions or highlight contributing factors.
-
Why it matters: Black-box algorithms undermine trust. Physicians need visibility into why a recommendation was made—especially in liability-sensitive specialties.
-
What to check: Heatmaps, confidence scores, explainable model layers, and traceable outputs.
For example: Paige AI shows heatmaps on pathology slides, helping validate its findings.
✅ 5. Data Privacy, Security & HIPAA Compliance
Ensure full HIPAA compliance and end-to-end encryption.
-
Why it matters: Medical data is among the most sensitive. Even well-intentioned AI tools can expose protected health information (PHI) if not properly secured.
-
What to check: Encryption protocols, local vs. cloud data handling, Business Associate Agreement (BAA) availability, and audit trail logging.
Don’t assume privacy just because the vendor uses “AI” – demand architecture-level clarity.
✅ 6. Transparent Limitations and Intended Use
The best tools are clear about what they do not do.
-
Why it matters: Medical AI tools are designed for narrow tasks (e.g. triage, flagging, decision support), not general diagnosis or autonomous decision-making.
-
What to check: Clear instructions for use (IFU), disclaimers, and clinical decision boundaries.
Ethical AI vendors will define use constraints; vague or overly broad claims are a red flag.
✅ 7. Proven ROI or Clinical Efficiency Gains
Look for evidence of real-world impact on outcomes, cost, or efficiency.
-
Why it matters: AI should either improve diagnostic accuracy, reduce clinician time, lower operational costs, or enhance patient throughput.
-
What to check: Customer case studies, peer-reviewed implementation data, or third-party ROI analysis.
Example: Clinics using Nuance DAX report up to 7 hours/week saved per physician in documentation.
✅ 8. User Training and Clinical Support
Successful adoption depends on training, onboarding, and continuous support.
-
Why it matters: Even great tools fail if end users aren’t equipped to use them confidently.
-
What to check: Vendor offers CME-accredited training, real-time clinical support, or EMR-integrated tooltips and decision guides.
Tip: Ask for references from departments already using the tool in similar settings.
Bottom Line:
AI in medicine must be held to the highest standards—comparable to pharmaceuticals or medical devices. Look for tools that are not only innovative but safe, proven, integrated, and clinically accountable.
-
-
Final Thoughts: Where Medical AI Is Heading Next
🧠 The AI-Driven Doctor Is No Longer a Vision—It’s Reality
From AI scribes reducing documentation time to imaging tools identifying strokes within minutes, medical AI is no longer experimental. It’s woven into daily clinical workflows—from solo practitioners to leading academic hospitals.
What’s changed in 2025 is that:
-
AI tools are now clinically validated and often FDA-cleared
-
Ease of use has skyrocketed—no more clunky integrations or data silos
-
Doctors are reclaiming time for patients, research, and well-being
🔬 What’s Coming Next in Medical AI?
-
Multimodal Models
AI tools that combine imaging, text, labs, and even genomics into one diagnostic suggestion. -
Real-Time AI Copilots in EMRs
Direct integration into Epic, Cerner, and Meditech—with voice-first inputs. -
AI-Driven Personalized Treatment Plans
Tailored therapy recommendations based on patient data, not population averages. -
AI-Supported Clinical Trials
Faster protocol generation, eligibility screening, and site matching.
✅ What You Should Do Now
-
If you’re in primary care or outpatient, test Glass AI or Nuance DAX Copilot to reclaim hours per week.
-
If you’re in radiology or acute care, prioritize Aidoc or Watson Imaging to enhance accuracy and triage speed.
-
If you’re in academic medicine or research, leverage BioGPT or PathAI to scale your output and precision.
You don’t need to become a tech expert—these tools were built for clinicians, not coders.
-
-
Expert Clarifications: What Doctors Ask About Medical AI
1. Are medical AI tools clinically validated, and to what extent?
Most leading diagnostic AI tools are validated through peer-reviewed studies, often using retrospective datasets. However, prospective, multi-center clinical trials remain limited. Always verify CE, FDA, or other regulatory clearances and check for published clinical performance metrics (e.g., sensitivity/specificity, AUC).
2. How accurate are AI diagnostic tools compared to experienced physicians?
In fields like radiology and dermatology, some AI systems have matched or exceeded average human performance in controlled settings. For example, Google's DeepMind has shown radiologist-level accuracy in breast cancer screening. But performance often drops in real-world clinical use due to data variability.
3. Which medical specialties benefit most from AI today?
Radiology, pathology, dermatology, ophthalmology, cardiology, and primary care have seen the most integration. Common uses include image analysis, triage, early detection, patient risk stratification, and automated documentation.
4. Are AI tools FDA-cleared or CE-marked for real-world clinical use?
Yes, several tools have FDA 510(k) clearance or CE marking (EU MDR). Examples include Aidoc (radiology), Viz.ai (stroke detection), and Eko (cardiology AI). Always verify clearance status and clinical indication before use.
5. Can AI legally be used to make autonomous medical decisions?
In most jurisdictions, AI tools are decision-support systems, not autonomous decision-makers. Final clinical judgment still lies with the licensed healthcare provider, per regulatory guidance and malpractice liability law.
6. What are the top legal and ethical concerns when using AI in patient care?
Major concerns include algorithmic bias, lack of transparency (black box), data privacy (HIPAA/GDPR), informed consent, liability in case of errors, and ensuring equitable care across populations.
7. How secure is patient data when using AI-powered apps?
Security varies widely. Only use tools that offer end-to-end encryption, HIPAA/GDPR compliance, anonymization or pseudonymization protocols, and transparent data use policies. Always vet vendors before adoption.
8. How does AI integrate into existing EMR/EHR systems?
Integration depends on the tool and the healthcare system’s interoperability. HL7, FHIR APIs, or vendor-specific modules are common. Some tools integrate directly with Epic, Cerner, or Allscripts systems. IT team involvement is crucial.
9. What is the liability if an AI tool makes an incorrect diagnosis?
Currently, liability still falls on the human provider. AI is a support tool, not a substitute for clinical decision-making. However, this legal landscape is evolving and will likely shift as AI use increases.
10. Are AI models biased against certain populations?
Yes, many early models underperform in underrepresented groups due to biased training data. Always check for studies showing demographic performance breakdowns, especially in tools involving imaging, vitals, or language input.
11. Can AI help reduce burnout in clinical practice?
Absolutely. AI-powered scribe tools, auto-charting systems, patient triage assistants, and automated prior authorization systems are helping clinicians cut down admin time and reduce cognitive overload.
12. How much training is needed to use medical AI tools?
Minimal training is usually required for front-end tools (e.g., diagnostic assistants, scribes). However, proper onboarding and understanding of limitations are essential. Some systems offer in-tool tutorials and CME-accredited onboarding.
13. Can AI tools be trusted with rare or complex conditions?
Generally, no. Most AI models are trained on large datasets that may underrepresent rare diseases or atypical presentations. Human oversight remains essential for complex or unusual cases.
14. What are the risks of AI “hallucinations” in clinical language models?
Medical LLMs can produce false or misleading answers that sound plausible—a phenomenon known as “hallucination.” Use tools that are trained on validated medical data (e.g., UpToDate, PubMed, clinical guidelines) and require user verification.
15. What should doctors look for when evaluating a new AI tool?
Key factors:
-
Regulatory status (FDA/CE/ISO)
-
Peer-reviewed clinical evidence
-
Real-world performance metrics
-
Transparency in algorithm function
-
Vendor reputation & security certifications
-
Ease of integration with workflow
⚠️ Final Reminder
All tools mentioned here are grounded in published validation studies, FDA status, or real clinical use. However:
Always review the privacy practices, HIPAA compliance, and integration pathways before deployment in a clinical environment.
Start small, measure the impact, and scale what works for your practice.
-
What's Your Reaction?
 Like
2
Like
2
 Dislike
0
Dislike
0
 Love
2
Love
2
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
2
Wow
2